02 Mar Foot Pain? Start at the back.
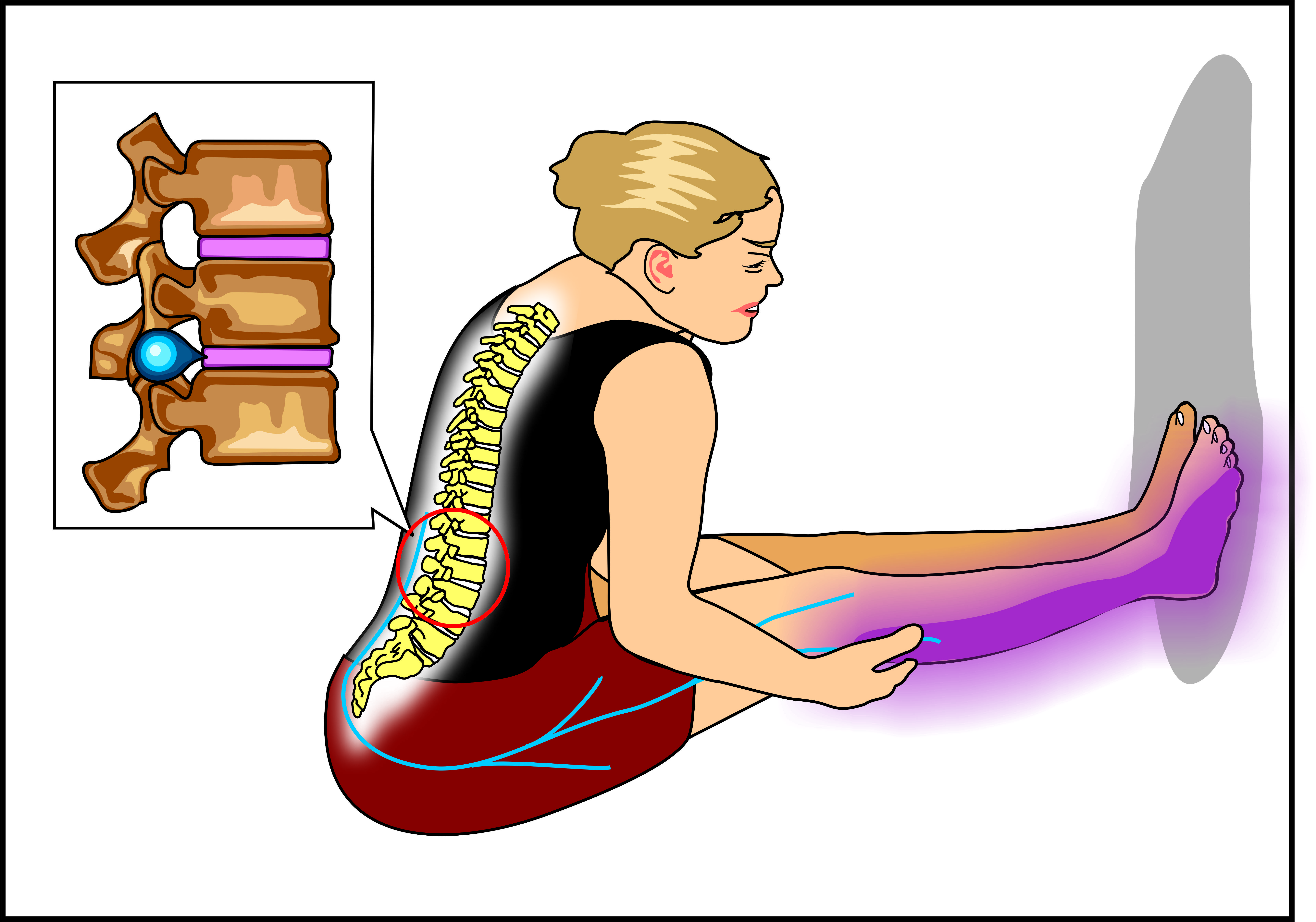
Where pain is and where it comes are in many instances two separate issues. Having a system to distinguish the two can be very important at getting to the root cause of a person’s condition.
The Importance of Systems
Systems are important because they allow you to break down complex and potentially dangerous situations into steps. It’s about stopping at a red light, and moving forward once you see a green one. Every successful person that works with analyzing complex situations works with a system. Same goes in physical therapy.
Systems Approach in a Physical Therapy
Although cases may have similar symptoms (e.g. low back pain), not every symptom has the same cause. Thus, it’s important to have a system to rule out all the potential dangers in order to come to a high probability treatment plan. The following is a real-life case:

Visit 1: Initial Evaluation
Step 1: Thorough Medical History
KB is a 43-year-old female with a prescription to evaluate pain in her right foot and big toe. Her pain started a few months ago of insidious onset (i.e. for no apparent reason). There is no trauma. She describes her right-side foot pain as achy and toe pain as throbby. Her pain rating is a 5/10 (10 = “have to go to the hospital”). She’s active and goes to her exercise class 3-4 times/week. It’s usually worse the next day after exercise and difficult to walk and push off her toes. It’s better with rest and when the foot is elevated. No other significant medical history except for left hip surgery to repair a torn labrum around 5 years ago.
Physical Therapist (PT) Thought Process so far
The first thing to do is take a thorough history. This gives us an idea of all the potential causes of KB’s symptoms and allows us to detect any “red flags”. These are clusters of symptoms (e.g history of cancer, unexplained weight loss, fever, redness, etc.), that, when presented together, need a referral back to the doctor. In this case, there are no red flags, so I feel pretty safe to continue the evaluation. I take note of her pain descriptions (“achy and throbbing”) and lifestyle (exercise class 3-4 times per week) and work towards my next step.
Step 2: Structural Exam
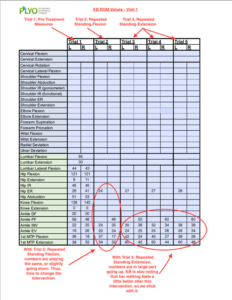
The second thing we want to do is see how KB’s body works as a whole and how pain is affecting it. For the most part, her walking looks good, however, we do notice that the right push-off of her gait is off. She rates walking a 5/10 pain on both the side of her foot and big toe. We note walking as her “functional baseline” and proceed to gather her “mechanical baselines” or range of motion values (ROM). (For the values we collected, see the table below. Visit 1 – Trial 1 = before any intervention or treatment).
Step 3: Directional Preference
The third step, after gathering baselines, is to determine if the spine is involved. For this purpose, we use Mechanical Diagnosis Therapy (MDT) or the McKenzie Approach. We have KB do 10 standing forward bends (or Trial 2 – Repeated Standing Flexion in the table above) to see the effect. We only re-measure numbers that are substantially different from the non-painful side.
PT Thought Process
When looking at the numbers after Trial 2, we don’t see any large increases in ROM. In fact, some are going down. So the next step is to see what happens when KB goes into another direction, backwards bends (or Trial 3 – Repeated Standing Extension, see picture below to see what it looks like).

After 10 backwards bends, we see that KB’s values are improving. Since the backwards bends are increasing KB’s ROM values, we ask KB to do 2 more rounds of 10 backward bends (Trial 4 and 5).
At the end of trial 5, we notice a consistent improvement in KB’s overall ankle and big toe ROM. We re-assess her pain with walking and it’s decreased from a 5/10 at the beginning of the visit to around a 4/10 at the end. Given her improvements in ROM and decrease in pain, we feel confident in giving KB backward bends as her homework and tell her to do 10 every hour.
Visit 2
KB comes into PT 2 days later feeling better. Her foot pain with walking decreased to a 2-3/10. However, her back is a little sore.
PT Thought Process
Even though KB’s back is sore, we know we’re on the right track because she’s feeling better overall. Before we start any treatment, we take a look at KB’s ROM values (See the table below. Visit 2 – Trial 1). When comparing Visit 1 to Visit 2, we do notice a decrease in lumbar flexion. However, her symptomatic R big toe (1st MTP flexion/extension) is better.

Our next step is to see KB do her homework (backward bends) and note whether her values continue to improve (See Table Above. Visit 2 – Trial 2). After 10 backward bends, we notice an overall increase in ROM. We’re on the right track. We decide to continue with 10 more backward bends (Trial 3). However, ROM is plateauing, so we decide to add a “force progression”. We have KB perform backwards bends from her stomach (see picture below). Her MTP flexion and extension (Visit 2 – Trial 4 and 5) values jump.

Conclusion
At the end of visit 2, KB’s pain with walking went down to a 0.5-1/10 compared to a 5/10 at the start of her initial evaluation. We feel confident with our treatment plan. Overall, although we’re seeing progress, we know we have much more work to do. By no means do we believe we’ve completely fixed KB’s issues. We just know her back was involved in her foot pain. In subsequent sessions, we know we’ll have to look further into our system and address side to side discrepancies. She’ll need to improve her overall strength, joint and nerve mobility, and muscle flexibility in order to minimize her chance of re-injury. For now, KB’s happy there’s pain relief in her R foot when she does exercises for her back. However, she knows the process of becoming “injury proof” is a process of its own.
This article is written by Dr. Ritchie Kim, PT, DPT, OCS, FAAOMPT. Ritchie is a Doctor of Physical Therapy, Board-Certified Specialist in Orthopaedic Physical Therapy and Fellow of the American Academy of Orthopaedic Manual Physical Therapy.

No Comments